This August celebrates National Immunization Awareness Month (NIAM). NIAM has been instrumental in helping state and local organizations increase awareness of the importance of immunization. It’s a great moment to look at the landscape – where we started, where we are, and where we need to be going.
Where we started

CDC headquarters, circa 1965, promoting immunization. Source: CDC
We’ve come a long way – immunization is the public health success story in our lifetimes. In the United States, vaccines have made once common diseases all but disappear. The 1950’s is often thought of as a “golden” time in the United States. But it wasn’t all good news. The 1952 polio outbreak in the US saw 57,628 reported cases. More than 3,000 people died and more than 21,000 were disabled from the disease [1]. In the 1950’s an average of 150,000 measles patients had respiratory complications and 4,000 patients had encephalitis each year resulting in 48,000 hospitalization annually [2].
But beginning in the second half of the 20th century, things changed. Numerous vaccines were licensed for use in the US:
1953: Tetanus and diphtheria (adult use)
1962: Oral polio vaccine (OPV) type 3
1963: Inactivated measles vaccine
Trivalent OPV
1971: MMR vaccine
In all, more than two dozen vaccines have been licensed to prevent diseases ranging from anthrax to yellow fever. But it wasn’t simply the ability to prevent once-deadly diseases that was a game changer, it was the community built to support awareness and improve access to vaccines that made the difference.
1963 saw the establishment of The Federal Immunization Grant Program, which provided funds for states to purchase vaccines and support immunization services. In 1993, Vaccines for Children program was established. These programs, and others, paved the way for the U.S. to significantly reduce the cases of many serious diseases.
Where we are
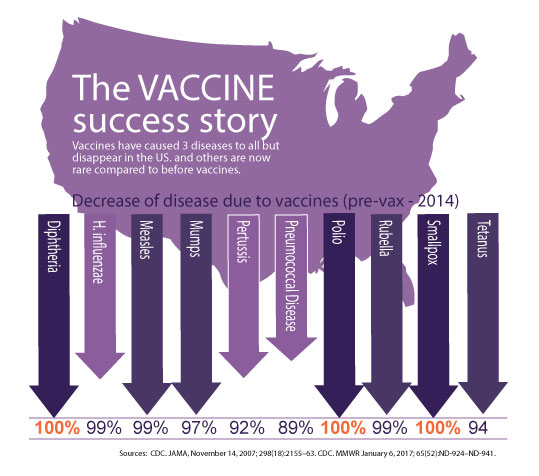 Today, diseases like diphtheria, polio and smallpox are unheard of in the U.S. Other diseases, like H. Influenzae, measles, mumps, rubella and tetanus are rare.
Today, diseases like diphtheria, polio and smallpox are unheard of in the U.S. Other diseases, like H. Influenzae, measles, mumps, rubella and tetanus are rare.
It’s a tremendous success story and we should all take a moment to reflect on that. The collective effort from scientists, public health advisors, and community organizers have all played a role is this success story. Organizations like the Rotary Club and National Foundation for Infectious Diseases have galvanized support that has changed the face of public health. Coalitions like the Immunization Action Coalition have provided support and resources to immunization advocates. State and local health departments have manned the front line for decades.
These partnerships have created a new reality in the U.S. – one where we no longer fear once dreaded diseases. And that’s amazing. But there is a darker side to this success. We now have generations that have never seen many of these diseases. And as result, doubt has started to creep in. Today, despite the evidence, despite the successes, there is an increase in vaccine safety concerns. While it continues to be a minority view, there is a troubling trend of questioning vaccine confidence.
So, as we celebrate the success of vaccines during NIAM, we should also be taking this moment to look forward.
Where we need to be going
Here are five issues that we need to focus on to ensure that immunization remains a public health success story:
1.Improving vaccination across the lifespan
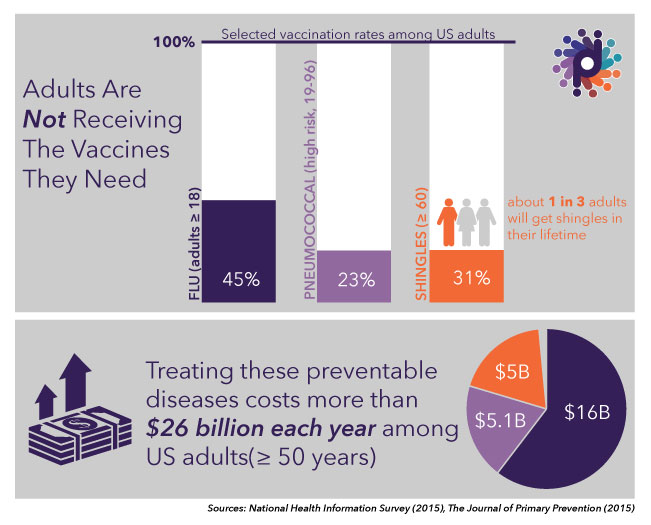 We’ve done an outstanding job with childhood vaccines, but many adults are not getting the vaccines they need. For example, only about 50% of adults get their flu vaccine each year, and only 20% of those 19-64 years at higher risk for complications from pneumococcal disease have received vaccination to protect against it [3]. The health and economic cost of vaccine-preventable diseases among adults is over $26 billion per year [4]. This will only increase as the U.S population continues to age [5].
We’ve done an outstanding job with childhood vaccines, but many adults are not getting the vaccines they need. For example, only about 50% of adults get their flu vaccine each year, and only 20% of those 19-64 years at higher risk for complications from pneumococcal disease have received vaccination to protect against it [3]. The health and economic cost of vaccine-preventable diseases among adults is over $26 billion per year [4]. This will only increase as the U.S population continues to age [5].
While older adults understand the importance of vaccines and there is coverage for them under Medicare, there is room for improvement in vaccination rates. For example, only 61.3% of adults 65 and older had received a pneumococcal vaccine in 2014 [6]. There are even more challenges in vaccination of adults under 65, who may not have health insurance, a regular source of health care, or realize they need vaccines.
Help adults understand what vaccines they need and address access / cost issues they may be facing.
2. Keeping an Eye on Global
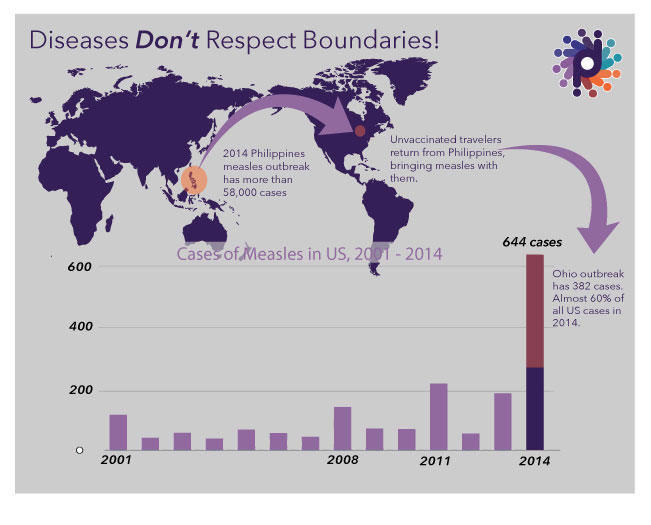
Diseases don’t respect boundaries. Other countries are working hard on immunization, and their coverage continues to grow, but they are not where the U.S. is yet. Some diseases that are rare in the U.S. are still common in other places. A more global world means diseases travel with people.
A 2014 measles outbreak infected hundreds in Ohio after two unvaccinated Amish men had returned from the Philippines, which was in the midst of an outbreak with more than 58,000 infections and 110 deaths. While this example shows the ease with which diseases can migrate, it also shows the power of partnership. A rapid and respectful response from the local health department, with support from CDC, saw a number of Amish families vaccinated in what had been a traditionally vaccine-reticent community.
Global doesn’t just mean disease travels…so do cultures and perceptions. Minnesota had more cases of measles in 2016 than all other states combined. The measles outbreak first occurred in the large Somali refugee population where vaccination rates are low (42% for Somali descent vs 89% for non-Somali descent). The low vaccination rates in the community were due to vaccine confidence issues. The State Department of Health has done a great job of engaging religious leaders and other trusted sources of information in the community. It has translated education materials into Somali and started a dialogue with the community around their concerns about Autism Spectrum Disorder [7]. It’s this thoughtful and culturally appropriate outreach that will help bolster confidence in unsure communities.
Keep an eye on global epidemics and have preparedness plans in place (including identifying vulnerable populations) should travel-imported cases come to your doorstep. Identify refugee / immigrant populations who may have specific information needs to make informed decisions.
3. Engaging the “Gray” Audience
Vaccines are often viewed as a black and white issue – you’re either for them or against them. But the truth is, there is a lot of shades of gray when it comes to vaccines. Recent studies suggest that up to 1 in 5 people have questions about the benefits and risks.
These people are not against vaccines; they are unsure. This is the “gray audience” – individuals, groups or communities that are searching for trusted information in order to make an informed decision.
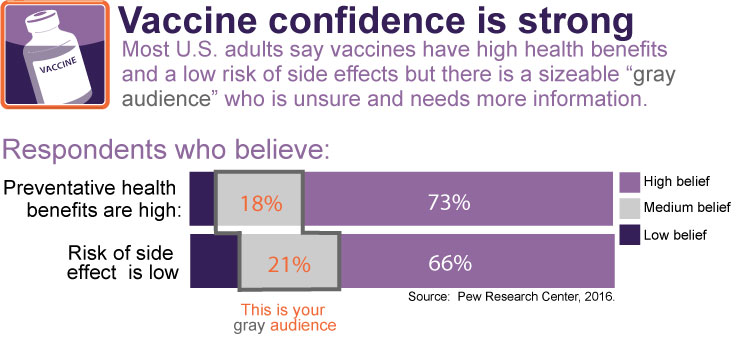
Gray audiences have many reasons for varying levels of confidence: religious, cultural, past experiences with health providers, etc. Each audience is likely to have slightly different motivators and barriers so take the time to 1) know who your gray audience is and 2) what their concerns are. Understand what they want to know and where they go for answers. Take an anthropological approach to understand how their perceptions are being shaped and socio-cultural issues you should be aware of when engaging them. And then make sure your messages respond to their concerns directly.
Take the time to understand your gray audiences, so you can help them to better understand vaccination benefits and risk to make independent, informed decisions.
4. Understanding the Role of Social Media
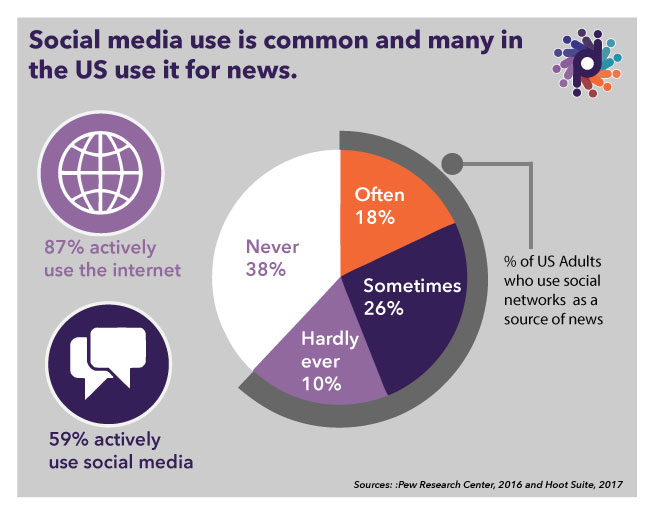
Social media is a great platform for engagement but can also be a double edge sword. Almost 70% of Americans use at least one social media site. While users skew younger, 60% of adults 50 – 64 and more than a third ≥65 do use social media [8]. According to the Pew Research Center, “personal contacts are also a common source of news and can play an amplified role online.” Stanford University and Pew Research Center have done research that shows both young and old have trouble identifying fact from fiction or identifying bias [9].Because social media is immediate, with the ability to amplify a message among personal contacts, this trend is very troubling. This presents a unique challenge to vaccine champions who can sometimes struggle to counteract “fake news.” Addressing this issue can seem like a lot of effort for already stretched thin advocates. But it’s an important issue and will only become more important as younger generations age, given social media is a mainstay of their information gathering.
Ensure you have a solid social media monitoring plan in place to identify trends and have a strategy ready so you can quickly and effectively address issues.
5. Building & Strengthening Partnerships
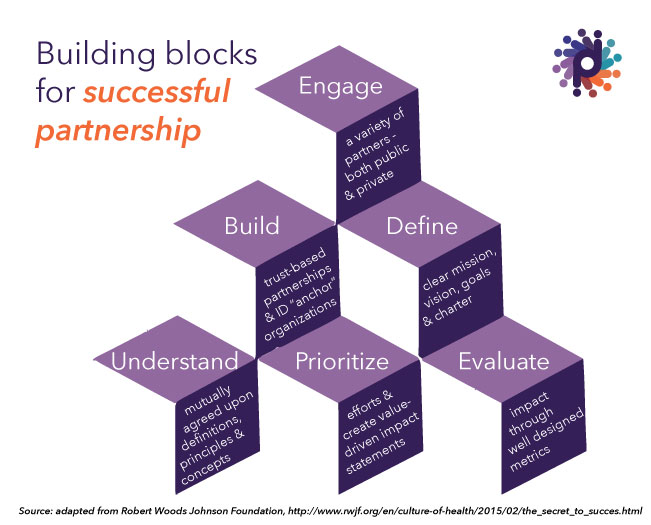 In real estate, the name of the game is location, location, location. In the world of immunization, it’s partnerships, partnerships, partnerships. Partnerships are what created the vaccine success story in the first place, and they are critical to its continuation. Build and grow them. Strong partnerships can share lessons learned, amplify messages, and provide access to hard to reach populations. But strong partnerships require a strong strategy and committed members to make them effective.
In real estate, the name of the game is location, location, location. In the world of immunization, it’s partnerships, partnerships, partnerships. Partnerships are what created the vaccine success story in the first place, and they are critical to its continuation. Build and grow them. Strong partnerships can share lessons learned, amplify messages, and provide access to hard to reach populations. But strong partnerships require a strong strategy and committed members to make them effective.
Get creative. Develop strong partnerships that can help you reach your priority audiences and strengthen focus areas. Invest in those partnerships to ensure they are effective and valuable to members.
This NIAM, let’s take time not only to celebrate our good work, but also to plan for success in the years to come.
Devi Partners has decades of immunization experience, working across the lifespan and around the world at local and national levels. For more information, visit www.devipartners.com.
___________________________________
References:
- Melnick J (1 July 1996). “Current status of poliovirus infections”. Clin Microbiol Rev. 9 (3): 293–300. PMC 172894 . PMID 8809461.
- Walter A. Orenstein, Mark J. Papania, Melinda E. Wharton; Measles Elimination in the United States. J Infect Dis 2004; 189 (Supplement_1): S1-S3. doi: 10.1086/377693
- https://www.cdc.gov/vaccines/vaxview/index.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4486398/
- https://www.census.gov/prod/2014pubs/p25-1140.pdf
- https://www.cdc.gov/mmwr/volumes/65/ss/ss6501a1.htm
- http://rtc.umn.edu/autism/
- http://www.pewinternet.org/fact-sheet/social-media/
- https://sheg.stanford.edu/upload/V3LessonPlans/Executive%20Summary%2011.21.16.pdf, http://www.journalism.org/2016/12/15/many-americans-believe-fake-news-is-sowing-confusion/